Many drugs are developed not because there's a great medical need, but rather there's big money to be made from them. In many cases, holistic therapies and medicines already exist that can take the place of any number of synthetic pharmaceuticals. Cannabis is one such therapy and it's time to ask questions and look at a new way of thinking about this plant, Dr Margaret Gedde, MD, PhD, Gedde Whole Health, Colorado, US, and the Clinicians' Institute of Cannabis Medicine, said. A wealth of research shows cannabis does indeed have outstanding promise as a medicinal plant, largely due to its cannabidiol (CBD) content. Cannabinoids interact with your body by way of naturally occurring cannabinoid receptors embedded in cell membranes throughout your body. There are cannabinoid receptors in your brain, lungs, liver, kidneys, immune system and more. Both the therapeutic and psychoactive properties of cannabis occur when a cannabinoid activates a cannabinoid receptor. About two years ago, Dr Gedde received her first request from a parent who wanted to use the high-CBD, low-Δ9-tetrahydrocannabinol (THC) form of cannabis for her child's epileptic seizures.
"I went ahead with that and started to learn about what this could do. Now, two years later, the news that cannabis is a therapy for epilepsy has reached the world. We're very committed to gather ongoing information about what's happening with these children and to get this information out to other physicians in a way that they can use and understand. We want to generate high-quality, publishable data from practice and our experience. We want to help people understand the background and the scientific basis of what cannabis can do and really start to understand that it's a medicine and bring it into what we have as medicine," she says.
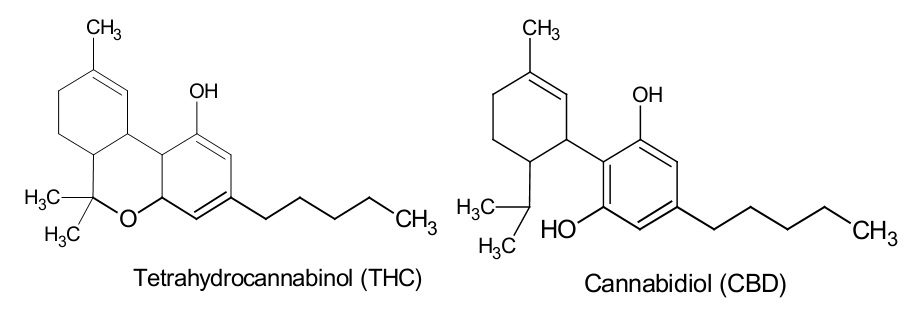 |
| THC and CBD molecules, showing their extremely close resemblance |
The cannabis plant contains many cannabinoids including CBD and THC. Both have medicinal properties; THC can cause psychotropic effects (feeling 'stoned'), CBD cannot. The whole plant contains a variety of terpenes that have varying medicinal properties too. Through traditional plant breeding and seed exchanges, growers have produced cannabis plants for medical use that have higher levels of CBD and lower levels of THC. Dr Allan Frankel, MD, one of the world’s leading authorities on dosed cannabis medicine (board-certified in California) who treats patients with medical cannabis, works with a number of CBD-rich strains.
In the US, CBD is currently a Schedule 1 controlled substance, (in Australia it is Schedule 9) which means, in the US:
- the 'drug' or other substance has a high potential for abuse,
- the 'drug' or other substance has no currently accepted medical use in treatment in the US,- the 'drug' or other substance has a high potential for abuse,
- there is a lack of accepted safety for use of the 'drug' or other substance under medical supervision.
 In Australia it means, under the Scheduling of Medicines and Poisons, Therapeutic Goods Administration (TGA):
In Australia it means, under the Scheduling of Medicines and Poisons, Therapeutic Goods Administration (TGA):- As a constituent of cannabis, the substance would be captured by the entry for cannabis in Schedule 9 (Prohibited Substance).
- CBD may also be a constituent of hemp seed oil ... defined as oil obtained by cold expression from ripened fruits (seeds) of Cannabis sativa and exempted from scheduling provided the oil contains 50 mg/kg or less of THC and is labelled with the warning statement: "Not for internal use" or "Not to be taken".
- CBD is mentioned in Schedule 8 (Controlled Drug) entry for 'nabiximols'* (defined as containing a range of cannabinoids including both THC and CBD).
Across the US there's no doubt that CBD needs to be rescheduled, as current scheduling is blatantly wrong. In Australia, an interim decision (on matters referred to an expert advisory committee, November 2014) to reschedule CBD (Schedule 4 - Prescription Only Medicine and Schedule 8 - Controlled Drug) was recommended by the Therapeutic Goods Administration (TGA) to be implemented 1 June 2015.
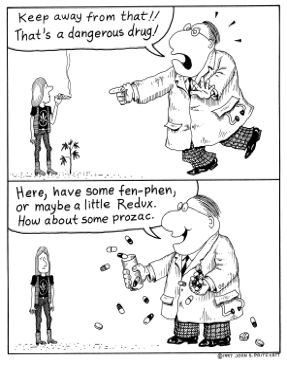
How Does Cannabis Compare to Prescription Drugs?
 A number of prescription drugs are well known to be dangerous. Pharmaceuticals in general are among the leading causes of death in the US and some drugs have killed tens of thousands of individuals. The painkiller Vioxx is one classic example that killed over 60,000 before being pulled off the market. In Australia the Royal Australian College of General Practitioners (RACGP) and the Pharmaceutical Society of Australia (PSA) had called upon Federal and State governments to implement a national Electronic Recording and Reporting of Controlled Drugs (ERRCD) system, after a Victorian coroner warned legal drugs were killing more people than illicit drugs or alcohol.
A number of prescription drugs are well known to be dangerous. Pharmaceuticals in general are among the leading causes of death in the US and some drugs have killed tens of thousands of individuals. The painkiller Vioxx is one classic example that killed over 60,000 before being pulled off the market. In Australia the Royal Australian College of General Practitioners (RACGP) and the Pharmaceutical Society of Australia (PSA) had called upon Federal and State governments to implement a national Electronic Recording and Reporting of Controlled Drugs (ERRCD) system, after a Victorian coroner warned legal drugs were killing more people than illicit drugs or alcohol.According to Dr Gedde, cannabis is certainly far safer than most prescription drugs and there's enough information to compare it against the known toxicities of many drugs currently in use. This includes liver and kidney toxicity, gastrointestinal damage, nerve damage and, of course, death. Moreover, CBD and other cannabis products often work when other medications fail, so not only are they generally safer, cannabis preparations also tend to provide greater efficacy. As noted by Dr Gedde:
"There's an ongoing death rate from use of pain medications as prescribed. So, even as prescribed, they're highly dangerous and they are open to abuse. As far as medications used in the paediatric population to control seizures, there are also severe toxicities to organs. Many of them are very sedating. The children become unable to function or really to interact because of the sedating effects. Other medications have a side effect of rage and behavioural problems. Unprovoked rage is actually a known side effect of some of the anti-seizure medications. Cannabis and in particular cannabidiol has none of these issues. No toxicities. The main side effect of cannabidiol is sleepiness. As a child gets accustomed to it, that does wear off and the child can be very alert and functional on the cannabis oil once they have worked into the dosing. Once you put them against each other, there really is no comparison in terms of safety."
Anti-epileptic Drugs (AEDs)
Epilepsy Action Australia defines anti-epileptic drugs (AEDs) as medications used in the management of seizures. Some forms of these medications are also used to treat neuropathic pain, bi-polar disorder and anxiety. Also called anti-convulsants and AEDs (please see list at the end of this article of current AEDs and some of their side-effects).
Cannabis for Seizure Control in Children
In Dr Gedde's experience, about 25% of children experience a rapid reduction in seizures when given cannabis oil, sometimes within days, or weeks. But results do vary, and not every child will respond well in the immediate term. She notes that some children are so sensitised to medications that they need to start at a very low dose, and give it plenty of time to work.
 "We are working out in the clinical practice the protocols that seem to give the best benefit the most quickly to the most children, but we do find that some children get results very quickly. For others, it takes more time, up to a number of months," she says.
"We are working out in the clinical practice the protocols that seem to give the best benefit the most quickly to the most children, but we do find that some children get results very quickly. For others, it takes more time, up to a number of months," she says.
There's limited information on using cannabis in children for issues other than epilepsy. However, in January 2015, the American Academy of Paediatrics (AAP) updated their policy statement on cannabis, acknowledging that cannabinoids "may currently be an option for … children with life-limiting or severely debilitating conditions and for whom current therapies are inadequate".
The main objection of paediatricians at the Children's Hospital in Denver to using CBD in children, even for conditions like uncontrolled seizures, is that there are no studies in children of potential harms of long-term use of CBD. There might be long term adverse effects of CBD and other cannabinoids that we will only come to discover later.
"This is a good point in my view, and a reason not to suggest use of CBD as a dietary supplement or as a general 'health tonic' for children", Dr Gedde says. "In my view, it is important to weigh the use of a therapy, including potential risks not known, against the risks of the uncontrolled illness itself and of other therapies in use. For many patients, even with incomplete information about CBD, weighing those risks including known toxic effects of their current therapies does point to at least a therapeutic trial with CBD being a good choice."
The main objection of paediatricians at the Children's Hospital in Denver to using CBD in children, even for conditions like uncontrolled seizures, is that there are no studies in children of potential harms of long-term use of CBD. There might be long term adverse effects of CBD and other cannabinoids that we will only come to discover later.
"This is a good point in my view, and a reason not to suggest use of CBD as a dietary supplement or as a general 'health tonic' for children", Dr Gedde says. "In my view, it is important to weigh the use of a therapy, including potential risks not known, against the risks of the uncontrolled illness itself and of other therapies in use. For many patients, even with incomplete information about CBD, weighing those risks including known toxic effects of their current therapies does point to at least a therapeutic trial with CBD being a good choice."
Potential Side Effects of Medical Cannabis
According to Dr Gedde the main side effect you need to watch out for is the psychotropic effects of THC. However, she also stresses that THC actually has many valuable medical benefits, so depending on your problem, you may want higher or lower levels of THC. For example, in patients who suffer with severe pain, where the perception of pain causes great distress, the psychotropic effects of THC allows the patient to shift their perception of the pain in their mind and body.
According to Dr Gedde the main side effect you need to watch out for is the psychotropic effects of THC. However, she also stresses that THC actually has many valuable medical benefits, so depending on your problem, you may want higher or lower levels of THC. For example, in patients who suffer with severe pain, where the perception of pain causes great distress, the psychotropic effects of THC allows the patient to shift their perception of the pain in their mind and body.
"That's an example where the psychoactivity is needed, but there are other areas where it's not. Selection of the type of product, the actual cannabinoids in it and the mode of using it is very helpful for dealing with that side effect," she says. "Beyond that and the kind of distress that excessive psychoactivity can cause if somebody gets too much, cannabis is very safe. There are no known deaths linked with it. That cannot be said about virtually anything else on the planet, including water. You can overdose on water and die. You can't get enough cannabis in your body to kill you."
 In Australia, Dr Andrew Katelaris, MD, UNSW, wrote in his submission to the Legal and Constitutional Affairs Committee with regard to the Inquiry into the Regulator of Medicinal
Cannabis Bill 2014;
In Australia, Dr Andrew Katelaris, MD, UNSW, wrote in his submission to the Legal and Constitutional Affairs Committee with regard to the Inquiry into the Regulator of Medicinal
Cannabis Bill 2014;
"I am one of a very few clinically trained medical professionals in Australia with experience in growing, extracting and administering cannabis medicines. Cultivars (cultivated varieties) of cannabis that are dominant in the non-psychotropic cannabinoid, CBD, have demonstrated dramatic effects in a subgroup of children with intractable epilepsy in overseas studies. Intractable epilepsy is, by definition, epilepsy that has not been controlled despite maximal combination therapy, leading to cumulative brain damage and early death of the afflicted child. Given the severity of their predicament and the impotence of the medical profession to assist, I prepared standardised extracts of a CBD dominant cannabis in medium chain triglyceride oil at a concentration of 5mg/ml and received volunteers requesting their child be included in this pilot study. Twenty children were administered this treatment, half the group being diagnosed with Dravet syndrome and the remainder having congenital, post infectious and post hypoxic aetiologies for their seizures. Approximately 80% of the recipients received benefit and all wished to continue with the medicine. No significant side effects were reported. In about half of the recipients, the benefit was nothing less than transformational. Not only was seizure activity reduced to a minimum or abolished, but the child's capacity for learning and skill acquisition, as well as social interaction was increased, in some instances dramatically. Repeated approaches have been made to the New South Wales (NSW) state government to reclassify CBD dominant cannabis as a medical herb, subject only to purity and potency control, without any reply or even acknowledgement being received. One can only hope that those considering this bill exercise their social conscience to a higher degree and take urgent action to enact this reclassification at a federal level. Not only does CBD have no psychotropic effect but it also negates the psychotropic effect of THC. Therefore, diversion is not an issue and cannot be used as an excuse to delay taking this necessary step."
Cannabis use in Australia is illegal no matter where you reside. State governments have promised trials of medical cannabis before the current plethora of purported 'medical cannabis' trials. The NSW Legislative Council, General Purpose Standing Committee No. 4 on 'The use of cannabis for medical purposes' recommended in May 2013
Cannabis use in Australia is illegal no matter where you reside. State governments have promised trials of medical cannabis before the current plethora of purported 'medical cannabis' trials. The NSW Legislative Council, General Purpose Standing Committee No. 4 on 'The use of cannabis for medical purposes' recommended in May 2013
"... in general terms medical cannabis has potential as an effective treatment for some medical conditions with appropriate safeguards in place [and] cannabis products are emerging as a promising area of medicine ..."
But for parents of children with intractable epilepsy it could be a case of too little too late and what parent could be blamed for risking that? One such parent, David Stevens writes;
"You should already know how strongly and passionately I feel about medicinal cannabis, especially what it has done for Deisha and many others. Now from the start I want to say that it may or may not work as well on your child as it has for Deisha, but every child with refractory epilepsy should have the opportunity to have access to medicinal cannabis and quite possibly give them and their families quality of life as well as possibly saving the child's life. It doesn't matter what level of government it is, nothing happens overnight and I applaud the governments in Australia who have taken positive action. Unfortunately with all the media attention that medicinal cannabis has been receiving this has led to limited supply and some unscrupulous people selling snake oil to desperate families. Now this is not acceptable and I don't want to see any child or family put at risk. The only answer I see for families to help their child now is to take control themselves.
GROW IT, MAKE IT, ADMINISTER IT!
So I've made a short video to show you how to make high CBD Medicinal Cannabis Oil for Paediatric Epilepsy to show families how easy and safe it is to make. No more meeting people late at night down dark lane-ways. You will now know exactly what you are giving your child. Please share to your hearts content." YouTube
As reported in The US National Library of Medicine (type the words 'cannabis epilepsy' in the search field and it will return nearly 800 very current results), one scientific study from 2010, Cannabidiol Displays Antiepileptiform and Antiseizure Properties In Vitro and In Vivo, states;
"Plant-derived cannabinoids (phytocannabinoids) are compounds with emerging therapeutic potential. Early studies suggested that cannabidiol (CBD) has anti-convulsant properties in animal models and reduced seizure frequency in limited human trials. CBD (100 mg/kg) exerted clear anti-convulsant effects with significant decreases in incidence of severe seizures and mortality ... Finally, CBD acted with only low affinity at cannabinoid CB1 receptors and displayed no agonist activity. These findings suggest that CBD acts, potentially in a CB1 receptor-independent manner, to inhibit epileptiform activity in vitro and seizure severity in vivo. Thus, we demonstrate the potential of CBD as a novel anti-epileptic drug in the unmet clinical need associated with generalised seizures".
Another study from 2013, Cannabidivarin (CBDV) suppresses pentylenetetrazole (PTZ)-induced increases in epilepsy-related gene expression, states;
"To date, anti-convulsant effects of the plant cannabinoid, CBDV, have been reported in several animal models of seizure. To examine changes to epilepsy-related gene expression following chemical convulsant treatment and their subsequent control by phytocannabinoid administration, we behaviourally evaluated effects of CBDV. Consistent with previous findings, CBDV significantly decreased PTZ-induced seizure severity and increased latency to the first sign of seizure. These results provide the first molecular confirmation of behaviourally observed effects of the non-psychoactive, anti-convulsant, cannabinoid, CBDV, upon chemically-induced seizures and serve to underscore its suitability for clinical development".
And a third study in 2013, Report of a parent survey of cannabidiol-enriched cannabis use in paediatric treatment-resistant epilepsy, states;
Severe childhood epilepsies are characterised by frequent seizures, neuro-developmental delays and impaired quality of life. In these treatment-resistant epilepsies, families often seek alternative treatments. This survey explored the use of cannabidiol-enriched cannabis in children with treatment-resistant epilepsy. The survey was presented to parents belonging to a Facebook group dedicated to sharing information about the use of cannabidiol-enriched cannabis to treat their child's seizures. Nineteen responses met the following inclusion criteria for the study: a diagnosis of epilepsy and current use of cannabidiol-enriched cannabis. Thirteen children had Dravet syndrome, four had Doose syndrome and one each had Lennox-Gastaut syndrome and idiopathic epilepsy. The average number of antiepileptic drugs (AEDs) tried before using cannabidiol-enriched cannabis was twelve. Sixteen (84%) of the nineteen parents reported a reduction in their child's seizure frequency while taking cannabidiol-enriched cannabis. Of these, two (11%) reported complete seizure freedom, eight (42%) reported a greater than 80% reduction in seizure frequency and six (32%) reported a 25-60% seizure reduction. Other beneficial effects included increased alertness, better mood and improved sleep. Side effects included drowsiness and fatigue. Our survey shows that parents are using cannabidiol-enriched cannabis as a treatment for their children with treatment-resistant epilepsy. Because of the increasing number of (US) states that allow access to medical cannabis, its use will likely be a growing concern for the epilepsy community. Safety and tolerability data for cannabidiol-enriched cannabis use among children are not available. Objective measurements of a standardised preparation of pure cannabidiol are needed to determine whether it is safe, well tolerated, and efficacious at controlling seizures in this paediatric population with difficult-to-treat seizures.
My personal opinion as an outsider looking in (I don't have a child with intractable epilepsy, thankfully) is that I would move mountains to help my child and these parents should never be criminalised for helping their sick and suffering children, never - the law is wrong in Australia and needs changed, now, not later, as later will be too late for some; and who would want that on their conscience? Exactly how much unnecessary paediatric poly pharmacy is involved with this disease alone is anyone's guess, but read on to learn just some of the nasty side-effects these real drugs have ...
Common Seizure Medication Side Effects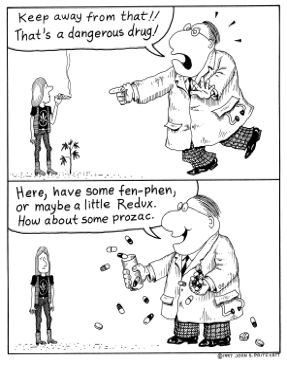 Seizure medications work on the central nervous system. Most cause some degree of drowsiness or dizziness, at least at the beginning of therapy. Also, most anti-seizure medications can induce suicidal thoughts or actions and/or bring on or worsen depression. Seizure medications have a variety of possible side effects. The following is a list of potential side effects of different classes of seizure medications.
Seizure medications work on the central nervous system. Most cause some degree of drowsiness or dizziness, at least at the beginning of therapy. Also, most anti-seizure medications can induce suicidal thoughts or actions and/or bring on or worsen depression. Seizure medications have a variety of possible side effects. The following is a list of potential side effects of different classes of seizure medications.
My personal opinion as an outsider looking in (I don't have a child with intractable epilepsy, thankfully) is that I would move mountains to help my child and these parents should never be criminalised for helping their sick and suffering children, never - the law is wrong in Australia and needs changed, now, not later, as later will be too late for some; and who would want that on their conscience? Exactly how much unnecessary paediatric poly pharmacy is involved with this disease alone is anyone's guess, but read on to learn just some of the nasty side-effects these real drugs have ...
Common Seizure Medication Side Effects
 Seizure medications work on the central nervous system. Most cause some degree of drowsiness or dizziness, at least at the beginning of therapy. Also, most anti-seizure medications can induce suicidal thoughts or actions and/or bring on or worsen depression. Seizure medications have a variety of possible side effects. The following is a list of potential side effects of different classes of seizure medications.
Seizure medications work on the central nervous system. Most cause some degree of drowsiness or dizziness, at least at the beginning of therapy. Also, most anti-seizure medications can induce suicidal thoughts or actions and/or bring on or worsen depression. Seizure medications have a variety of possible side effects. The following is a list of potential side effects of different classes of seizure medications.
Acetazolamide (Diamox): Kidney stones, Increased urination, Loss of potassium
Benzodiazepines (Valium, Ativan, Klonopin, Onfi): Dependence, Possible severe seizures on sudden withdrawal, Respiratory depression, Increased risk of glaucoma, Liver injury
Carbamazepine (Tegretol) and related drugs: Upset stomach, Serious (even fatal) skin reactions, Serious blood disorders, Reduced sodium levels (oxcarbazepine)
Ethosuximide (Zarontin) and derivatives: Serious blood disorders
Ezogabine/Retigabine (Potiga): Potentially irreversible eye damage, Potentially irreversible skin discolouration
Felbamate (Felbalol): Liver failure, Potentially fatal anaemia (aplastic anaemia)
Gabapentin (Neurontin): Weight gain, Behavioural changes including hyperactivity
Lacosamide (Vimpat): Skin rash, Changes in heartbeat with possible fainting, Drug dependence
Lamotrigine (Lamictal): Serious rash, Stomach problems, Difficulty sleeping
Levetiracetam (Keppra, Keppra XR): Headache, Flu-like symptoms, Weight loss, Changes in behaviour, Changes in blood count
Perampanel (Fycompa): Severe changes in mood and behavior, including hostility, aggression, suicidal thoughts, Weight gain, Drug dependence
Phenobarbital and derivatives: Birth defects, Memory loss, Depression
Phenytoin (Dilantin): Body hair growth, Birth defects, Gum disease, Seizures with higher doses
Pregabalin (Lyrica): Swelling of hands and feet, Trouble concentrating, Weight gain
Rufinamide (Banzel): EKG changes, Interference with oral contraceptives
Tiagabine (Gabitril): Tremour, Agitation, Seizures in non-epilepsy patients
Topiramate (Topamax): Increased risk for glaucoma, Trouble concentrating, Decreased sweating, Increase in body temperature
Valproic acid and derivatives (Depakene, Depakote): Stomach upset, Temporary loss or thinning of hair, Pancreatitis, Toxicity to liver, Weight gain, Birth defects
Vigabatrin (Sabril): Irreversible visual problems, including reductions in acuity and colour differentiation
Zonisamide (Zonegran): Kidney stones, Rise in body temperature, Metabolic acidosis
Benzodiazepines (Valium, Ativan, Klonopin, Onfi): Dependence, Possible severe seizures on sudden withdrawal, Respiratory depression, Increased risk of glaucoma, Liver injury
Carbamazepine (Tegretol) and related drugs: Upset stomach, Serious (even fatal) skin reactions, Serious blood disorders, Reduced sodium levels (oxcarbazepine)
Ethosuximide (Zarontin) and derivatives: Serious blood disorders
Ezogabine/Retigabine (Potiga): Potentially irreversible eye damage, Potentially irreversible skin discolouration
Felbamate (Felbalol): Liver failure, Potentially fatal anaemia (aplastic anaemia)
Gabapentin (Neurontin): Weight gain, Behavioural changes including hyperactivity
Lacosamide (Vimpat): Skin rash, Changes in heartbeat with possible fainting, Drug dependence
Lamotrigine (Lamictal): Serious rash, Stomach problems, Difficulty sleeping
Levetiracetam (Keppra, Keppra XR): Headache, Flu-like symptoms, Weight loss, Changes in behaviour, Changes in blood count
Perampanel (Fycompa): Severe changes in mood and behavior, including hostility, aggression, suicidal thoughts, Weight gain, Drug dependence
Phenobarbital and derivatives: Birth defects, Memory loss, Depression
Phenytoin (Dilantin): Body hair growth, Birth defects, Gum disease, Seizures with higher doses
Pregabalin (Lyrica): Swelling of hands and feet, Trouble concentrating, Weight gain
Rufinamide (Banzel): EKG changes, Interference with oral contraceptives
Tiagabine (Gabitril): Tremour, Agitation, Seizures in non-epilepsy patients
Topiramate (Topamax): Increased risk for glaucoma, Trouble concentrating, Decreased sweating, Increase in body temperature
Valproic acid and derivatives (Depakene, Depakote): Stomach upset, Temporary loss or thinning of hair, Pancreatitis, Toxicity to liver, Weight gain, Birth defects
Vigabatrin (Sabril): Irreversible visual problems, including reductions in acuity and colour differentiation
Zonisamide (Zonegran): Kidney stones, Rise in body temperature, Metabolic acidosis
expanded from Cannabis for the Treatment of Epilepsy and More
with additional information from Granny Storm Crow's List 2015, Google Scholar
 funded NPS MedicineWise
funded NPS MedicineWise
*Sativex®